
A few of us at Core recently participated in HMPS25 in Orlando. It’s always inspiring to immerse our minds and hearts in the latest conversations in the healthcare marketing industry and learn from the experiences of our extraordinary clients, strategic partners and new connections. My only regret is that it’s impossible to go to every single session, which I absolutely would if I could!
Several key themes stand out:
- There was a lot of talk about AI, as you would expect; these sessions offered inspiration to more fully embrace AI as a “magical copilot” and supportive augmentation for all kinds of applications.
- There was vigorous conversation about value-based care and payviders as these models are picking up steam in the industry.
- An uplifting session about brand differentiation through unified storytelling inspired marketers to “Break the Brand Blur.”
- The gathering grappled with addressing the needs of younger and older consumers.
- The urgent need to build trust was a major through thread.
AI: A Magical Copilot
AI can be a “magical copilot,” according to keynote speaker Amber Mac. She spoke about the need to adapt to living in “predictable unpredictability,” adopting AI that helps you achieve your long-term purpose and developing an AI stack, adapting to new tools along the way.
Mac shared her favorite AI tools with the audience:
Perplexity: For research (I agree, this is a favorite for me, too)
Opus: Quickly makes short video clips from longer video content
Omnisend: A free email subject line tester
NotebookLM: Can use text to create a podcast-like conversation
HeyGen: Real-time translation of video to other languages (The speaker’s mouth adjusts to move according to the new language which is pretty slick!)
In another keynote, Tom Lawry encouraged the audience to see AI as an important healthcare tool, not as a threat.
“If you choose to lean in, you’ve got this.”Tom Lawry - Author of Hacking Healthcare and Healthcare Nation
Lawry said that AI will augment and not replace marketers. AI adds value in two ways — automating highly repetitive activities and augmenting activities that are more highly varied and require a higher level of problem solving. Lawry recommended that we each figure out how to bring AI in behind us to do the things we do best.
In healthcare, he noted that physicians are increasingly using ambient listening to take notes during patient visits, thereby freeing up themselves to be fully present with patients and reducing clinician burnout. He also shared some truly revolutionary examples, including AI taking a single chest x-ray and predicting 10-year stroke risk, and computer-aided diagnosis of diabetic retinopathy.
For healthcare marketing, he focused on applications including precision outreach to patient segments by condition, behavior or risk; predictive engagement and retention by forecasting no-show and service needs; and content and health literacy personalization. He gave the example of one healthcare marketer using AI to translate a complex clinical report to a patient handout at the fourth-grade reading level — in 15 minutes.
Value-Based Care and The Rise of the Payviders
The industry is coming to terms with ever-shrinking margins and the CMS (Centers for Medicare and Medicaid Services) push towards value, with more systems piloting programs and therefore healthy discussion of the model at HMPS25.
In a session called “Strategic Priorities in Healthcare: The Outlook,” Andrew Taylor from AdventHealth and John Fink and Dave Willis from ECG Management Consultants highlighted the uncertainty of governmental regulation, with the ubiquitous media narrative constantly shifting the blame for systemic problems to health systems.
They recommended focusing on what systems can fix now that consumers are focused on — primarily access, better experience and better outcomes — which the value-based care model addresses. In the absence of a population health-based model, there will be an inherent misalignment between mission and financial performance, according to the presenters.
“Health systems that bear risk, offer patient-friendly physical and virtual care settings, and invest in data analytics will be the ones that will prove relevant and achieve their visions.”Strategic Priorities in Healthcare: The Outlook - HMPS25
Health systems must practice balanced vertical integration by becoming payviders and offering wellness services, according to the presenters.
A panel discussion featuring speakers from Hartford Healthcare, UPMC Health and Mass General Brigham also focused on payviders as “a growing force in healthcare.”
Mike Sweeney from UPMC Health expressed his belief that, “If you focus on quality and clinical opportunity, the finance will come. When the industry gets to value-based care — and it will — it’s going to impact everything.”
They discussed that VBC will continue to grow as there is much more incentive now — and fee for service margins are not coming back.
If value-based care and population health are topics of interest to you, check out our ebook, Building Your Brand Around Population Health Strategy.

Breaking the Brand Blur
Skip Hidlay, Chief Communications & Marketing Officer at The Ohio State Wexner Medical Center and Ryan Donohue from NRC Health presented one of my favorite sessions, with a combination of interesting research and simply beautiful brand storytelling.
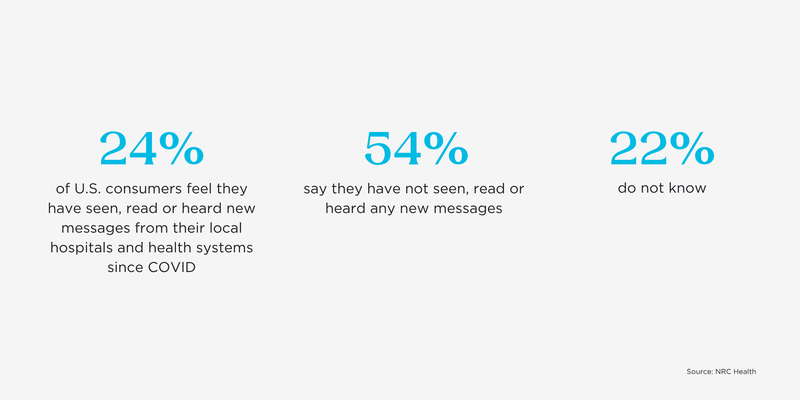
NRC’s research indicates that patients have a “foggier” view of healthcare than before the COVID-19 pandemic, which is consistent with other marketing research on the topic. According to their presentation, “Our pandemic response blended traditionally competitive voices together and included hospitals, insurers, health departments, politicians, charities, local groups, activists, etc. and consumers tuned in. Our collective show of unity left behind a blur of brands: consumers fusing brands together and becoming less likely to tell them apart. Important to remember: effectively reaching consumers and differentiating from competitors has been tough for a while.” I think we all know this intuitively; and yet, seeing the NRC data with its minuscule perceived differences between brands is still startling, because it doesn’t have to be that way.
NRC stated that healthcare brands have failed to send fresh, unique messaging to their communities. In fact, they asked consumers, “Since COVID do you feel you’ve seen any new messages from your local hospitals and health systems?” Only one in four (24%) said yes. Donohue also noted an “explosion in the lack of brand preference,” with 30% of consumers having no preference whatsoever.
Hidlay, The Ohio State marketing leader, shared his substantial team’s solution for “breaking through the brand blur” — the Ohio State “Health & Discovery” storytelling platform and flagship content engine, through which they unite communications. Their content strategies focus on filling gaps in high-search content, positioning their experts as content authors, and using deep storytelling to highlight innovative people and programs.
Their work is beautiful in its simplicity and touching in its empathy, as in this patient story about a boy who — under their care — recovered the use of his arm. I also admire their willingness to use a little humor, as in this patient story about a brother and sister with aortic dissection.
Innovating for Younger and Older Consumers
In a keynote session, Amber Mac presented data indicating that young people in Generation Z spend a whopping 109 DAYS on their screens each year. If anyone was still thinking that traditional primary care is the front door for most of them, this was a wake-up call. The majority prefer virtual care, and we need to work together to engage them in new and innovative ways. We need to make mental and behavioral health services more accessible, so they have options beyond relying on ChatGPT as their daily therapist, as Mac indicated that many are. She also highlighted the need to lead with your purpose (or, in Simon Sinek-speak, “start with why”), as “nearly all Gen Z want purpose-driven experiences and they are not afraid to turn down experiences that don’t align with their values.”
Multiple sessions focused on the growth of the older adult population and the need to innovate to better meet their needs. A session presented by Ellen Dalton and Lisa Slama from VillageMD focused on the fact that in value-based primary care, older adult engagement is paramount to success. With one in five Americans turning 65+ by 2030 and one-third of adults 65+ struggling to afford Medicare premiums, medications and care, to say the U.S. healthcare system is under pressure is a gross understatement.
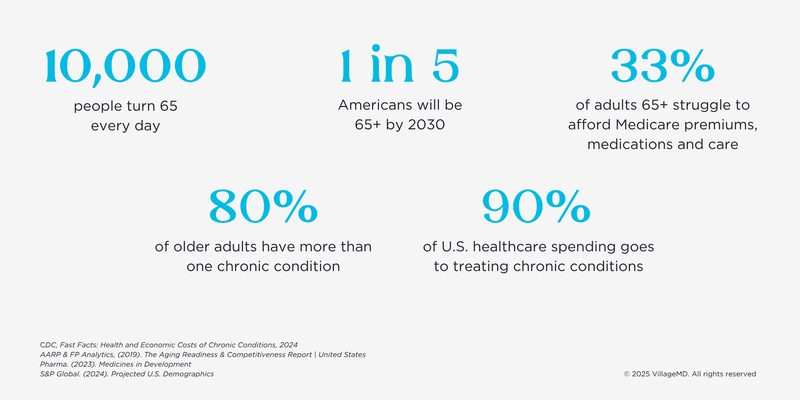
As the presenters noted, accountable care and value-based care models need to keep older adults as healthy as possible, avoiding high cost to the system, high misery to people and communities, avoidable ED use and hospitalizations, and missed quality benchmarks. I love this quote they shared from Dr. Zenobia Brown, their Chief Clinical Officer: “The bar is high for value-based primary care for older adults: we must provide exquisite care at every moment.” Now *that* is where the bar should be set for care.
Separately, Mike Yost and Jeremy Rogers from Indiana University Health shared their experience prioritizing change for older adults, along with Kellie Bliss from Merge. They are defining innovation priorities such as a trial on pre-dementia screening, care at home, and building a health district which they described as “the largest healthcare construction project in the Western hemisphere.” They spoke openly about a failed value-based care trial in which they did not have the density of patients (in a more rural area) to support Medicare-only clinics; however, they are not abandoning the VBC model, because they “still believe that value-based care is the answer.”
The Trust Imperative
Throughout the conference, from session to session, the need to build more trust in various ways showed up again and again.
Research findings presented by Jarrard put the shortage of trust into sharp focus:
- Trust that hospitals put patients over profits has dropped by more than 50 points since the pandemic.
- As of January 2025, only 24% of consumers surveyed believe that hospitals in the U.S. are mostly focused on caring for patients, while 76% believe that hospitals in the U.S. are mainly focused on making money.
- As a thin silver lining, people feel significantly more positive about hospitals and their own healthcare than the system in general (though still not wildly positive), according to the same research.
- Also, trust in doctors and nurses for health information has barely wavered; they remain the most trusted source for information about medical and health issues, over hospitals, the CDC and public health officials.
In the end, HMPS25 was a passionate reminder that everything we do — whether it’s using AI, building value-based care, differentiating our brands, caring for younger and older consumers in the ways that they need, or countless other things — should be about building trust with our consumers and team members. I feel hopeful that the growth of value-based care and population health in particular will go a long, long way towards helping us all build that trust.
Download now
A big takeaway from HMPS25 is that population health and value-based care continue to be priorities — and they don’t always get the spotlight they deserve in healthcare branding.
Our new eBook, Building Your Brand Around Your Population Health Strategy, is a practical guide for healthcare marketers and strategy teams who want to bring more visibility, purpose and clarity to their work.
Inside, you’ll learn how to:
- Bring clarity to population health and value-based care messaging
- Better connect your strategy with brand storytelling
- Get inspired by real-world campaigns and insights from leaders like Mark Clement, CEO of TriHealth