
Five healthcare landscape shifts & how marketers should respond.
Trends come and go in the healthcare industry. Each year, hundreds of articles are published about the next big thing and its anticipated impact. But while trends may pass, there’s often a bigger, broader landscape shift driving them from behind the scenes.
These shifts can happen gradually, slowly changing the market and trickling down into the individual trends we see today. Or they can be massive, earth-changing disruptions that turn entire industries upside down.
Some of the landscape shifts we’re experiencing have been expected for years, others are relatively surprising. Either way, as a marketing leader, you have to skate to where the puck is going, not where it currently is. Whether you represent a major health system, a smaller healthcare organization, or a B2B company, your willingness to think outside the box and prepare for uncertain future events will empower your organization to withstand the heavy winds of change.
What are the Biggest Landscape Shifts in the Healthcare Industry?
The past few years have seen plenty of anticipated as well as sudden landscape shifts within the healthcare industry. And the ramifications have usually been severe. Since the pandemic first put strain on healthcare systems, leaders, employers, workers, and patients have wondered when (or if) we ever will get back to "normal."
But “business as usual” is a bygone era in healthcare. These landscape shifts are creating a disruptive, competitive environment. They mean leaders must act with more innovation, more creativity, and ultimately, more empathy.
The most pressing landscape changes happening right now all revolve around care: access and delivery. It’s no longer enough to care for patients in a strictly clinical way. Rather, it’s imperative that healthcare systems and organizations figure out how to care for the whole person now more than ever. Here’s why.
1. Your patient demographics are changing
Across the country, the makeup of who you’re marketing to and caring for is changing. Baby boomers, one of the largest generations, are growing older. This has the potential to overwhelm health systems and cause major disruption for caregivers. In addition, the racial demographics of communities are evolving and becoming more diverse. Black, AAPI, and Hispanic populations are growing and will make up the majority of communities within the next two decades.
Those assertions probably aren’t that surprising to you. Neither of these shifts are new. In fact, these changes were predictable and well-documented. But just because you see change on the horizon doesn’t always make it easier to plan for the situations ahead.
A large aging population will almost certainly put a strain on the healthcare environment, and more diversity will require a different approach to traditional healthcare staffing and delivery, as well as marketing and advertising.
Key considerations
Innovation in care is paramount to serving an aging population. Senior living facilities, home care, and even surgical innovations and medical devices can help increase the quality of life for elderly people. For example: joint replacements used to be a difficult surgery with a long recovery process, but new surgical innovations make weight-bearing possible almost immediately after surgery. This enhances the quality of life and can help people live pain-free, get back to an active life, and require shorter hospital stays and less aftercare.
For changing demographics, access and equity are vital. Keeping a pulse on the communities your healthcare organization serves will help you better understand the needs of your consumers, patients and families. Changes as simple as ensuring your communications are available in multiple languages can have a big impact on the people you serve.
2. People are moving
While demographics are shifting, so too is the geographic landscape. Many people relocated during the pandemic with some choosing to make their new locations permanent. Others began settling outside major metro areas in search of the space suburban or rural settings offer.
This initial, dramatic, nationwide exodus from cities has created new challenges for healthcare planning and infrastructure — namely, the people you serve might be farther away. For regular check-ups and elective procedures, this might not pose too much of a problem. But for emergency services, what happens when a large population now lives 90 minutes from the nearest trauma center?
Key considerations
Long-term strategic planning (or real estate acquisitions) can’t happen in isolation. In partnership with your community, insurance providers, and other stakeholders, consider how you can reach the consumers who rely on your health system. It could be deciding where to place new facilities or outpatient centers, or even considering how to provide effective digitally-enabled healthcare through telemedicine and other new technology.
3. Caregivers are in short supply
Nursing shortages made headlines throughout the pandemic. Many healthcare professionals are experiencing burnout and post-pandemic PTSD. In fact, it’s estimated that 47% of healthcare workers in the U.S. plan to leave their jobs in the next few years. This will undoubtedly squeeze remaining nurses and caregivers even more.
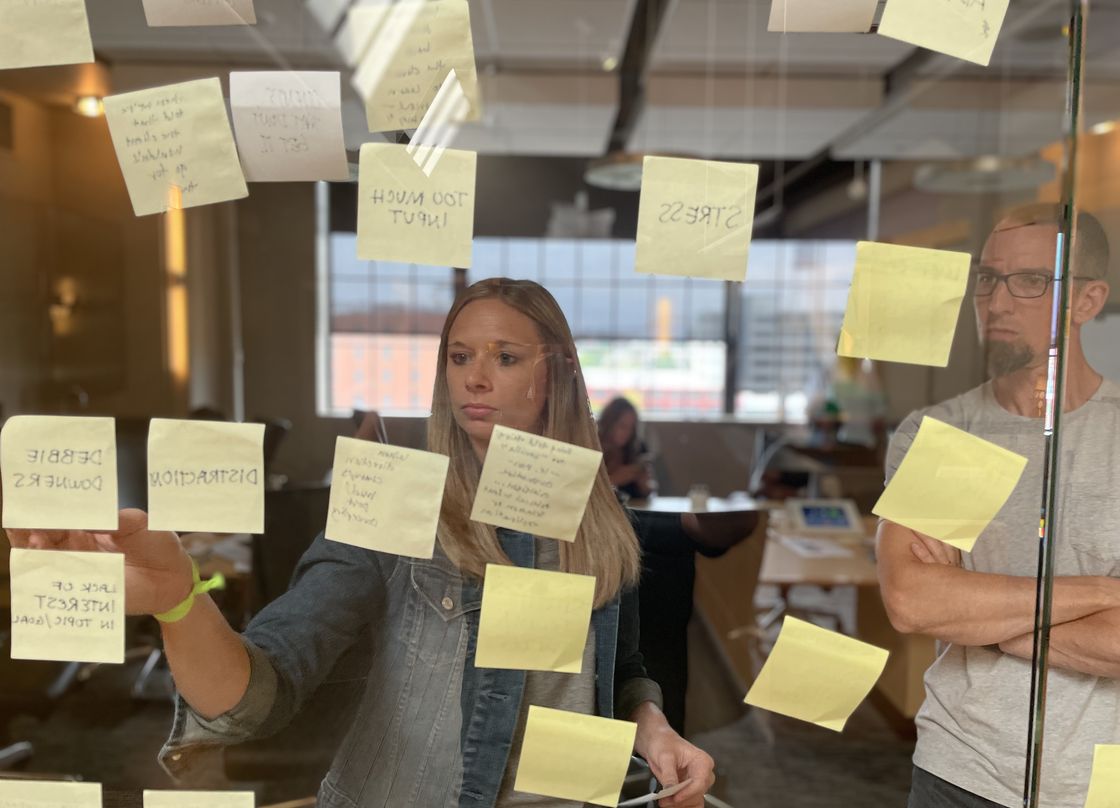
Despite this looming crisis, much of the current thinking around recruiting and retaining employees still revolves around one-time signing bonuses or “perks” such as lunches or branded apparel. But those are expensive and ineffective solutions to the already-apparent and long-term staffing shortages.
Key considerations
Short-term solutions like hiring bonuses aren’t sustainable. Instead, make a sustained effort to invest in your workforce. A supportive work environment, generous benefits, and competitive wages are just the starting point (and often table stakes). After that, you need to consider how this landscape shift is converging with others. An aging population will demand more and different sorts of caregiving services. And you can rest assured that new entrants to your market will come with innovative solutions for home care.
There’s an opportunity to differentiate yourself, not just as an employer, but as an innovator in the caregiving space by tapping into creative expertise and thinking about nontraditional paths that reduce the strain on caregiving staff. For example: remote patient monitoring might allow more older folks to comfortably age in place, while still having access to the care and assistance they need, rather than uprooting their lives to move into an assisted living facility. These innovations may require strategic partnerships to effectively and efficiently address the coming challenges.
4. Climate change has health implications
Climate change is a divisive issue — the political landscape in our country has led to skepticism and in some cases denial. But unfortunately, climate change causes health issues that can’t be ignored.
Natural disasters exacerbated by extreme weather are causing immediate and long-term health risks. For example, climate change has led to hotter and drier conditions for longer periods of time throughout the country. This has led to more and more wildfires. Putting the ecological impact aside, wildfires have an enormous impact on air quality — over time that can impact health.
Key considerations
Climate change is going to affect your community’s needs. Regardless of the ongoing debate, hospitals can take steps to reduce their own carbon footprint — like seeking renewable energy sources, prioritizing eco-friendliness in the supply chain, or even using reusable or compostable dishes over styrofoam plates and plastic utensils.
Beyond that, look ahead and see where your health system, products, or services can mitigate the healthcare industry’s impacts of climate change. Plan how your hospital will handle climate emergency situations. What happens if the power goes out for an extended period of time? What if ambulatory services can’t reach your emergency department because of flooding? Mitigating risk can also be actionable, not just hypothetical and preventative. For instance, if you operate in an area heavily impacted by fires, make asthma testing accessible and recommend it earlier for children and adults experiencing symptoms.
5. The healthcare industry has been politicized
Climate change isn’t the only divisive issue affecting the healthcare industry at a macro-level. Healthcare itself has become a polarized topic. It’s dangerous that the shifting landscape is also shifting the public perception and level of trust of healthcare systems and services. And as with climate change, people (including your patients or customers) have become suspicious (at worst) and skeptical of scientific and medical experts.
The resistance and subconscious biases consumers and patients hold make it harder for health systems and companies to effectively communicate with their target audiences. We’re seeing some consumers resist new healthcare innovations due to distrust, fear, anxiety, or an abundance of caution. Others seek information based on confirmation bias, the concept that people only accept information that suits their preconceived ideas, making them more likely to reject the factual information they don’t like. Both situations require healthcare marketers to educate or reassure their patients — especially when misinformation campaigns actively give audiences a more palatable, albeit factually incorrect, alternative to life-saving medical advances.
Key considerations
The bottom line is to educate rather than dictate, and to treat patients with empathy and humility. Educating patients and guardians on the best possible outcomes of preventative medicine or procedures is more likely to succeed than trying to change opinions through combative messaging.
This was our guiding principle when we worked closely with our client, Arkansas Children’s, to jumpstart conversations around vaccinating children for COVID-19. We relied on a strategic approach built on trust and reassurance as the best path forward. We knew that rather than creating a directive, it was important to give their audience tools to make the most informed decisions based on scientific evidence. And together, we helped Arkansas Children’s launch a statewide campaign that increased child COVID-19 vaccination rates by 14%.
Broad Implications for the Entire Healthcare Industry: Live Your Values for Success
The market is moving faster than ever, patients are being bombarded with conflicting messaging, and healthcare systems are facing financial pressure. That means you’ll have to respond with creativity, innovation, and out-of-the-box thinking as your first step to clearly differentiate your organization.
And these shifts require more than just innovation. It’s no longer enough to have digitally-enabled infrastructure or cutting-edge solutions. Every healthcare brand will be doing the same eventually. Sure, doing it first might give you a leg up, but for sustainable, continued success, you have to lead with empathy.
When you think about your place in the market, not just as a company or healthcare system, but as humans, you can begin to identify ways to make real emotional connections with your audience. By living your company’s values, you’ll be able to create authentic messages that tell the story patients need to hear — whether it’s to assuage concern about a new treatment, comfort the loved ones taking care of their elderly parents, or get ahead of long-term health implications of smoke and smog.
The industry will always change, but one aspect will remain constant: at the heart of healthcare are people. Because of that, empathy is the most essential factor in creating a connection between your brand and your audience, no matter the shifts in the landscape.